- Ultrasonic therapy is the therapeutic application of ultrasound waves within
the frequency range between 0.7 MHz to 3.3 MHz with energy absorption at a depth of 2 to 6.5 cm of soft tissue. Used to promote tissue healing and decrease pain in both acute and
chronic conditions.
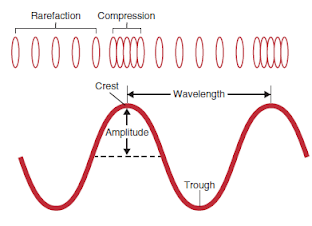
- Ultrasound is a form of acoustic vibration or mechanical vibration propagated in the form of longitudinal compression waves, at frequencies too high to be heard by the human ear.
- Frequency of Sound waves:-
 |
- Majority of Ultrasound generators are set at a frequency of 1 MHz but some units are set at 3 MHz.
- Ultrasonic energy generated at 1 MHz transmitted through the more superficial tissue and absorb primarily in deeper tissues up to 2 to 6.5 cm.
- At 3.3 MHz, the energy is absorbed up to 1 to 2 cm of penetrated tissue.
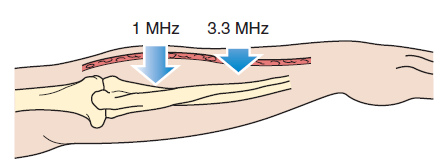
Frequency controls the depth of penetration of ultrasound; 1 MHz ultrasound penetrates approximately 3 times as far as 3.3 MHz.(picture adapted from Cameron, fourth edition)
PRINCIPAL OF ULTRASONIC THERAPY
Ultrasonic therapy transfer high-frequency sound pulse in the body by using a probe to produce the thermal and mechanical effect in the tissues. Recently it was found that it also has the non-thermal effects.
- Thermal effect:- The continuous transfer of ultrasound waves from transducer head to tissue generates a considerable amount of heat which absorbed by tissue causing an increase in tissue temperature results in a chemical equilibrium of tissue,which is helpful in the removal of scar, deep tendon healing etc.
- Non- thermal effect:- On and off the transfer of ultrasound results in the dissipation of heat during the off-time, causing an increase the intracellular calcium level and cell membrane permeability, facilitate tissue healing, modify inflammation and enhance transdermal drug delivery.
- Piezoelectric effect:- when certain crystals such as quartz, tourmaline, zirconate titanate and signette's salt are put under stress and released alternatively, a potential difference is produced across their faces and they change their shape. This phenomenon is called the piezoelectric effect.
- Reverse piezoelectric effect:- A condition, when crystals are under the influence of high-frequency alternating current, they compress in size and when the current is off they expand.
- In Ultrasonic generator, the reverse piezoelectric effect is used, where compression and expansion of the crystal hitting the front metal plate causing vibration and produces ultrasound waves.
- The source of high-frequency current is conveyed by a coaxial cable to the transducer circuit and to treatment head or applicator or sound head.
- Inside the transducer circuit, high-frequency current is applied to the crystal, that being fused to the metal front plate of the treatment head.
- Change in Crystal shape causes vibration of the front metal plate which in turn produce ultrasonic waves.
- Strict frequency control of high-frequency current (1 MHz to 3 MHz) ensures a steady and regular rate of deformation.
TRANSMISSION OF ULTRASOUND
- Ultrasonic waves are a series of mechanical compression and rarefaction of air particles in the direction of the waves, hence called the longitudinal wave.
- Air does not transmit Ultrasonic waves because of its less elastic nature, as being a longitudinal wave sound needs a medium to travel. So great care is needed to be taken to not leave air between the treatment head and patient.
A. REFLECTION:-
 |
| Ultrasound reflection and refraction. (picture adapted from Cameron, fourth edition) |
- When ultrasound beam passes through one medium to another, there will be a certain amount of reflection occur preventing the complete transmission of ultrasound waves, this reflection depends on the acoustic impedance (z) of the medium.
- Acoustic impedance is the ratio between the reflected and transmitted Ultrasound at an interface. How deep an ultrasound beam passes through tissue depends on the resistance provided by the tissue. this physical property of tissue resistance described as acoustic impedance.
1. Reflection at transducer head- skin interface:- when head and skin are not in proper contact, a small air pocket remains between them causing reflection of Ultrasound to the transducer head. Which lead to damage to the piezoelectric crystal and may cause excessive heating of the transducer head and skin.
2. Reflection at the tissue - air interface:- Occur when ultrasound is given to the thin area such as the palm of the hand where Ultrasound goes through the tissue and then meet the air opposite side. Pain felt in the area of the skin opposite the transducer head.
3. Reflection at bone periosteum:- At bone periosteum, 70% of energy is reflected and 30% is absorbed by the bone. As the Ultrasonic energy is absorbed in the periosteum, it quickly heats up causing periosteal pain.
- When Ultrasonic beam encounters an interface between the two media and transmitted, it may be refracted i.e. deviated from its path.
- While travelling from a medium with low velocity to a medium with high velocity, ultrasound beam deviates away from its target path.
- It describes the gradual reduction of Ultrasound intensity once left from transducer head and reaching towards the target site.
- Factors which contribute to attenuation:-
- The overall effect of these is that the Ultrasonic beam is reduced in intensity, the deeper it passes.
- This gives rise to the term "Half value distance".
- Half value distance:- The depth at which half of the initial energy has been absorbed.
- The deeper the energy penetrates into the tissues, it decreases exponentially, as a proportion of it, is absorbed in each unit distance.
- The half-value distance for 1 MHz is 6.5 cm and 3 cm for 3 MHz.
- No beam of Ultrasound emitted from the transducer head come out uniformly even in a homogeneous medium.
- The Beam Non-Uniform ratio (BNR) is used to find the average non-uniform nature of Ultrasound beam.
BNR = The spatial peak intensity/The spatial average intensity in the beam.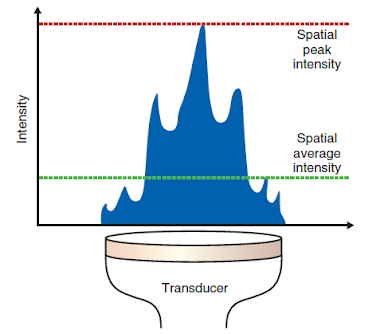
Beam nonuniformity. (picture adapted from Cameron, fourth edition) - Spatial peak intensity:- The peak output intensity of an ultrasound beam at one point over the area of the transducer head.
- Spatial average intensity:- The average output intensity of an ultrasound beam over the area of the transducer head.
- At only one point in the centre, the intensity is at its peak, regardless at minimum over the edges of the transducer head.
- The lower the BNR, more uniformly the beam travel across the transducer head, prevent high-intensity hot spots and tissue damage.
- Near field:- Is the region up to which ultrasound beam converge.
- Far-Field:- Is the region from where the ultrasound beam starts diverging.
- The depth of the near field varies with the frequency of Ultrasound. The extent of the near field depends upon the radius (r) of the transducer head and the wavelength (ƛ) of the ultrasound beam in the medium. The depth of near field= r²/ƛ
- Ultrasonic Waves are not transmitted by air, that's why a couplant is used in between transducer head and skin.
- Air reflect the ultrasound beam back into the treatment head, which might damage the crystal.
- Consequently, the treatment head should not be left switched on, when not in contact with a medium.
- No couplant affords perfect transmission of ultrasound waves and only a percentage of the original intensity is transmitted to the patient.

- Acoustic impedance is similar to the tissue, which does not let the reflection to occur.
- High transitivity for Ultrasound, which let the ultrasound to travel deeper.
- High viscosity, let the media to stay not to drop off.
- Low susceptibility to bubble formation, to decrease the chances of cavitation.
- A chemically inactive nature.
- Hypo allergic character.
- Relative sterility.
- Cheap.
- Act as a lubricant to allow the treatment head to move smoothly over the skin.
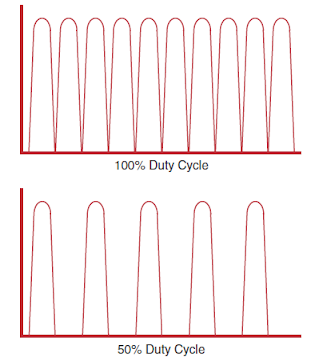
- Continuous mode:-
1. Continuous transmission of Ultrasound waves throughout the treatment.
2. This mode produces a thermal effect and used for musculoskeletal conditions such as muscular spasm, joint stiffness, pain etc. - Pulsed mode:-1. Transmission of ultrasound occurs in intervals, not continuously during the whole treatment.
2. When the transmission occurs it called on time and when it stopped, it called as off time.
3. The pulse mode produces less heat so it is used for soft tissue repair. Eg, Tendinitis.
- Amount of ultrasonic energy transmission during the treatment depends on the intensity of ultrasound and duration of treatment, and every condition requires a different amount of ultrasonic energy.
- Duration of treatment depends on the Size of the affected area, generally, 1-2 minutes for every cm² id recommended.
- Minimum- 1-2 minutes
- Maximum- 8 minutes
- Average- 5 minutes
- For chronic- longer treatment time
- For acute - lesser treatment time.
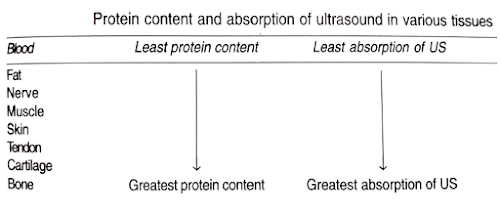
- The absorption of ultrasound waves in the tissues results in oscillation of the particles. this oscillation produces heat, which is proportional to the intensity of the ultrasound waves.
- The amount of heat generation within the tissues depends on the heat absorption by tissues and the amount of heat which is not dissipated.
- The heat absorption by tissues depends on the following factors which are as:
- Pressure changes applied to tissues by the ultrasound waves produce certain effects without increasing the temperature of the tissues, these are known as Non-Thermal effects.
- Non-thermal effects achieve by using the pulsed mode where mark: space ratio is 1:2, 1:4 and 1:8 is seen at minimum.
- The physical mechanism which is involved in producing these non-thermal effects are:
- When bubbles oscillate to and fro within the Ultrasonic pressure waves but remain intact.
- While oscillating through many cycles, micro-scale eddy currents are produced around these oscillating bubbles known as micro-streaming.
- Micro-streaming:- micro-scale eddy currents produced around oscillating bubbles causes reversible permeability changes in cell membrane locally. for example, increase the permeability of calcium ions and enhances cell activity.
- Occurs when the volume of bubbles increases rapidly and collapse suddenly.
- It is dangerous to the tissues as the collapse of the bubbles causes a high-pressure change and great local rise in temperature, leads to the free radical formation and gross tissue damage.
- It is avoided by moving the treatment head (to prevent standing waves), using a space average intensities (below 4 watts/cm²) and using a pulsed mode.
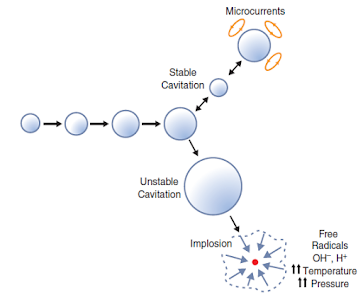 Cavitation and microstreaming. (picture adapted from Cameron, fourth edition)
Cavitation and microstreaming. (picture adapted from Cameron, fourth edition)
- This occurs when the longitudinal compression waves of Ultrasound beam produces compression and rarefaction of cells and affect the tissue fluid movement in the interstitial space.
- Helps in reducing oedema
- Combining with thermal effect, this makes it easier to stretch the scars and adhesion by affecting their extensibility.
- Inflammatory:-
Ultrasound interact cells of repair process such as platelets, micro-phages, mast cell by producing platelet permeability and increasing intracellular calcium ions which eventually helps in releasing histamine by degranulation. - Proliferative:-
1. Ultrasound affects the rate of angiogenesis.
2. Enhance the motility and proliferation of fibroblast cells which produces collagen fibres and synthesis protein and eventually leads to wound contraction. - Re-modelling:-
Increase the extensibility and tensile strength of scar by affecting the direction, strength and reducing the cross-linking of collagen fibres.
Schematic Diagram of the Effects of Therapeutic Ultrasound. (picture adapted from Therapeutic Modalities, fourth Edition)
- Ultrasound helps in breaking of adhesions formed between adjacent layers, thus removes the chronic oedematous fluid. for example in chronic traumatic oedema in the ankle.
 |
Ultrasound is applied to the posterior knee in conjunction with an extension stretching force. (picture adapted from Cameron, fourth edition) |
- Immobilization, inactivity and scarring cause limitation in joint ROM and limitation of function. e.g. shortening Joint capsule, surrounding tendons or ligament.
- Using this modality will increase the temperature of soft tissue and it's extensibility, makes it easier to stretch.
- As these tissues have a high ultrasound absorption coefficient which makes it, a good modality to use in such condition.
- Stimulates the cutaneous thermal receptors and inhibit pain by the pain gate mechanism as well as enhancing the soft tissue extensibility when using continuous mode.
- it's a viral cutaneous infection causing skin lesions containing thrombosed capillaries covered by hyperkeratotic epithelial tissue, occurring commonly in plantar surfaces of children or young adults.
- Recent studies show that the use of ultrasound modality will decrease these lesions at 0.6-0.8 W/cm², a continuous mode for 7-15 minute with 2-15 treatments.
- Recent injuries and inflammation:- As discussed in biological effects, ultrasound helps in removal of tissue exudates and promotion of tissue repair which leads to inflammation resolution and pain reduction. example sprain and strain.
- Calcium resorption:- Ultrasound helps in resorption of calcium deposits from certain tendons such as over supraspinatus tendon.
- Bone fracture healing:- Recent studies recommended ultrasound parameters 0.15 w/cm², pulsed 20% duty cycle, 1.5 MHz frequency applied for 15-20 minutes, is useful in efficient fracture healing.
- Surgical incision healing/ scar tissue:- Ultrasound is applied on first or second postoperative days for gynaecological surgical wounds and episiotomies in human, have been found to reduce pain, and resolve the haematoma which enhances breaking strength of such wounds.
- Herpes Zoster infection pain:- For the treatment of pain resulting from acute herpes zoster low dose ultrasound is recommended.
CONCLUSION
- Ultrasound is
used as a therapeutic modality in physiotherapy to decrease pain and promote
healing in both acute and chronic injuries. Mostly used frequencies in clinical
practice are 1 MHz and 3 MHz. Ultrasound waves with 1 MHz frequency penetrate
deeper than the 3 MHz.
- Apart from frequency,
intensity and duration of using ultrasonic waves also vary with the
condition.
- Ultrasonic
waves can produce thermal effects when applied continuously and non-thermal
therapeutic effects when given in pulsed mode, it depends on the condition
which mode should be used. Generally, in acute injury pulsed mode and in
chronic pain continuous mode of ultrasonic therapy is used.
- There are
specific properties of Ultrasound like reflection, refraction, attenuation and
absorption which determines the transmission of ultrasonic waves in turn guide
the way of using it in therapeutic setup, by some terms like acoustic
impedance, half value distance and BNR etc.
- Therapeutic ultrasound produces many thermal and non-thermal effects, which can be used to treat many conditions ranging from acute injuries to chronic pains.
Resources
· Electrotherapy Simplified – Basanta Kumar Nanda
· Clayton’s Electrotherapy: Theory and Practice, eighth edition – Forster & Phalastanga
· Physical Agents in Rehabilitation: From Research to Practice, fourth Edition -Michelle H. Cameron
· Textbook of Electrotherapy, second edition – Jagmohan Singh
· Physical Principle Explained – John Low and Ann Reed
· Therapeutic Modalities, fourth Edition - Chad Starkey
· Ultrasonic Therapy – Physiopedia







1 Comments
Nice
ReplyDeletePlease do not enter any spam link in the comment box