Passive Knee Stabilizers are non-contractile structures like the joint capsule, ligaments and menisci etc. Which stabilize our knee joint and help in arthrokinematic of knee joint
In our previous post (click here), we discussed "how our knee joint work". But that was only bony movement and we know that bone can not move by itself, we need some active (muscle) and passive (capsulo-ligamentous) stabilizers which stabilize our knee joint and help in knee joint motion.
In this, we are going to study only about "Passive Knee Stabilizers"
MENISCI
- The medial and lateral menisci are fibrocartilaginous structures located within the knee joint.
- The medial meniscus is "C" shaped and Lateral meniscus is almost "circular".
- The medial meniscus is less mobile due to greater ligamentous and capsular restraints than the lateral meniscus.
 |
| Fig 1.1 Superior view of tibia showing menisci and cruciate ligament (adapted from Neuman, 2nd edition) |
- The menisci convert the articular surface of the tibia into the concave surface for the convex femoral condyles.
Functions:-
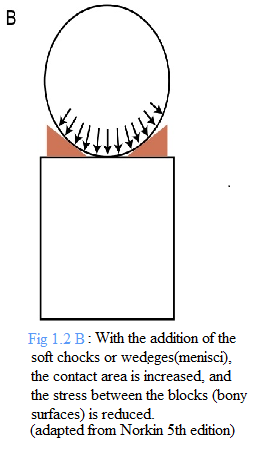
- The primary function is to reduce the compressive stress across the tibiofemoral joint by distributing weight-bearing forces (Fig 1.2).
- Reduce friction between the tibia and femur
- Stabilize the joint during motion
- Act as a shock absorber
- Improve joint congruency
- Facilitate normal joint arthrokinematics
- Provide proprioception
Meniscal nutrition and Innervation
- The periphery part is vascular(obtain its nutrition through a blood vessel) but the inner part, in contrast, is essential, avascular.
- Innervated by free nerve endings(nociceptors) and three different mechanoreceptors (Ruffini corpuscles, panician corpuscles and Golgi tendon organs).
Clinical relevant
- Due to the avascular nature of the inner part of menisci, reduce the potential for healing after an injury.
- Proprioceptive deficits occur, as a result of injury to the mechanoreceptors within the meniscus.
- Removal of menisci(meniscectomies), increase the joint stress (multiplies the forces by six or seven times on the tibial plateau) and may lead to damage of the articular cartilage, which contributes to degenerative changes within the tibiofemoral joint.
- The medial meniscus is injured twice as frequently as the lateral meniscus due to relative lack of mobility of medial meniscus, has greater ligamentous and capsular restraints than the lateral meniscus.
Joint capsule
 |
| Fig 1.3 Showing both the layers of the joint capsule. |
- The joint encloses both tibiofemoral and patellofemoral joint.
- It's composed of 2 layers:-
b) deep thin synovial layer
- secrete and absorb synovial fluid into the joint
( B) Fibrous layer
- support to a joint is provided by the several capsular thickenings or (capsular ligaments) (Fig 1.4).
- Anteriorly, anterior portion of the knee joint capsule is called extensor retinaculum.
- Medially, the thickest band ( transverse oriented fibres)within the medial retinaculum is the medial patellofemoral ligament.
- Laterally, fibres(transverse oriented fibres) within the lateral retinaculum called a lateral patellofemoral ligament.
- The remainder of the retinacular bands includes the obliquely oriented medial patellomeniscal ligament, the lateral patellomeniscal ligament and longitudinally positioned medial and lateral patellotibial ligaments.
- Posterior joint capsule reinforced by posteromedially by oblique popliteal ligament, posterior oblique ligament, and posterolaterally by arcuate ligament, lateral collateral ligament, popliteus muscle/tendon (Fig 1.5).
 |
Fig 1.4 Anterior view of knee, showing reinforcement of extensor retinaculum by medially and laterally ligaments. ( adapted from Norkin, 5th edition) |
 |
| Fig 1.5 A view of the posterior capsule of the knee. ( adapted from Norkin, 5th edition) |
Function:- Both the posterior oblique ligament and the arcuate ligament, assist in checking the hyperextension of the knee.
Innervation:- Innervated by both nociceptors as well as mechanoreceptors( Pacinian and Ruffini corpuscles).
Anterior and Posterior cruciate ligament
- Both ligament cross each other within the intercondylar notch of the femur, Connect tibia to the femur.
- Both are the important "passive knee stabilizers", in the sagittal plane.
- Both are intracapsular but extra synovial.
- Both cruciate ligaments innervated by the mechanoreceptors
- consist 2 separate bundles:
a) anteromedial bundle (AMB)
b) posterolateral bundle (PLB)
- When the knee close to full extension, the PLB is taut & AMB is relaxed.
- As the knee flexes, AMB becomes tight & PLB is relaxed.
- The shift in the tension between the bundles, allow some portion of the ACL to remain tight at all times (Fig 1.7)
Functions:-
1. The primary function is Resist anterior translation of the tibia on the femur (open chain kinematic) and posterior translation of femur on the tibia (closed chain kinematic).
2. Resist hyperextension of the knee.
3. Resist extreme of valgus, varus and axial rotation.
4. In addition to stabilizing the knee, contribute proprioception to the knee as they contain mechanoreceptors.
5. Guide the natural arthrokinematic of the knee joint.
- consist of 2 separate bundles
a) anterolateral bundle (ALB)
b) posteromedial bundle (PMB)
- When the knee close to full extension, the PMB become taut & ALB is relaxed.
- As the knee flexes, ALB becomes taut & PMB is relaxed.
Functions:-
1. The primary function is to resist posterior shear of the tibia on the femur (open chain kinematic) and anterior shear of the femur on the tibia (closed chain kinematic).
2. Resist extreme of valgus, varus and axial rotation.
3. In addition to stabilizing the knee, contribute proprioception to the knee as they contain mechanoreceptors.
4. Guide the natural arthrokinematic of the knee joint.
Medial and Lateral Collateral ligament
 |
| Fig 1.8 Anterior view of knee, showing medial and lateral collateral ligament. |
- Both ligaments are the important "passive knee stabilizers", in the frontal plane.
(A) Medial collateral ligament (MCL)
- a broad structure that crosses the medial side of the knee joint.
- It has 2 portions:-
- The superficial portion is longer, it arises proximally from the medial femoral condyle travels distally to insert into the medial aspect of the proximal tibia.
- A deep portion is shorter, it arises from the inferior aspect of the medial femoral condyle, continuous with the joint capsule travel distally to insert into the medial tibial plateau and rigidly affixed to the medial border of the medial meniscus.
Functions:-
- The primary restraint to excessive valgus at the knee.
- Resist excessive lateral tibial rotation at the knee.
- Secondary role as a restraint to anterior tibial translation.
- As it taut in full extension, assist with locking the knee.
(B) Lateral collateral ligament (LCL)
- Cross the lateral side of the knee joint.
- Proximally arise from the lateral femoral condyle travel distally to the fibular head, where it joins with the tendon of the biceps femoris muscle.
Functions:-
- The primary function is to resist varus stress at the knee.
- Resist excessive lateral tibial rotation at the knee.
- As it taut in full extension, assist with locking the knee.
(C) Clinical Relevant
- As Medial collateral ligament(deep portion), attached to the medial joint capsule and medial meniscus, severe injury to medial collateral ligament involve medial joint capsule and medial meniscus also.
- Simultaneous Injury to the medial collateral ligament, the medial meniscus and anterior cruciate ligament called "terrible triad"(O' Donoghue triad) of knee joint structure.
Till now, we cover the "passive knee stabilizers" individually and their functions. Now we will study their role in arthrokinematic of the knee joint.
Role of Cruciate ligaments and Menisci in Arthrokinematic of knee joint
- Cruciate ligaments
1. During weight-bearing knee flexion, anterior cruciate ligament gets taut and creating an anterior translational force on the femoral condyle (Fig 1.9 A) 2. During weight-bearing knee extension, posterior cruciate ligament creating a posterior translational force on the femoral condyles (Fig 1.9 B) |
1. During weight-bearing knee flexion, the oblique contact force of the menisci-on-femur(MF) guide the femur anteriorly during flexion, while the reaction force of the femur-on-menisci(FM) deforms the menisci posteriorly on the tibial plateau (Fig 1.10) |
2. During weight-bearing knee extension (return to extension from full flexion), the posterior deform menisci return to their neutral position.
Conclusion:
In this post, we studied about the Passive Knee Stabilizers.
"Passive Knee Stabilizers" are joint capsule, ligaments and menisci.
Initially, we studied all these, individually what are they? What are there functions?
Like, some increase joint congruency, act as a shock absorber, distribute weight, provide proprioception and the structure which provide frontal and sagittal knee stability.
After that, we studied how these Passive Knee Stabilizers help arthrokinematic of the knee joint,
like During knee flexion, PCL guide femoral condyle to translate anteriorly and menisci deform posteriorly to translate femoral condyle on the relatively fixed tibial plateau.
Reference article
For more in details please click the reference link down below.
Resources
1) Joint structure and function, a comprehensive analysis 5th edition by Pamela K. Levangie, Cynthia C. Norkin
2) Kinesiology Of Musculoskeletal System, foundations for rehabilitation 2nd edition by Donald A. Neuman









0 Comments
Please do not enter any spam link in the comment box